Does combining two evidence-based exercise programs in elderly people with incontinence have a triple effect on incontinence symptoms, balance and functional status?
Improving pelvic floor muscle training (PFMT), balance and functional activity is recommended in the treatment of urinary incontinence (UI) in the elderly people. The aim of this study is to examine whether PFMT combined with Otago exercises is effective on symptoms, balance and functional status in elderly people with UI compared to PFMT alone.
Methods
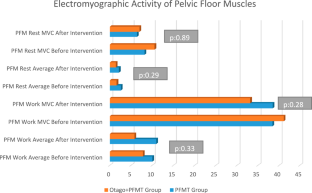
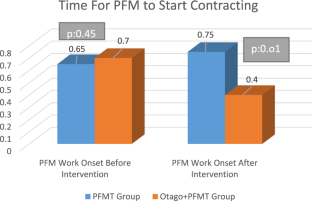
This study is an assessor-blinded, randomized controlled trial. Participants with UI aged 65 and over living in a nursing home were randomly assigned to the intervention (IG) and control groups (CG). The intervention group attended an exercise program that included Otago exercises combined with PFMT. The control group was included in the PFMT program with different positions. The duration of exercise for both groups was 45–60 min per session three times a week for 12 weeks. UI symptoms and severity (Pelvic Floor Distress Inventory-20, bladder diary), PFM muscle function (superficial electromyography), balance (Berg Balance Scale), functional status (Senior Fitness Test) and fear of falling (Falls Efficacy Scale) were measured at baseline and after the intervention.
Results
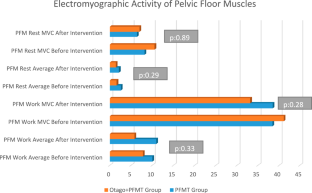
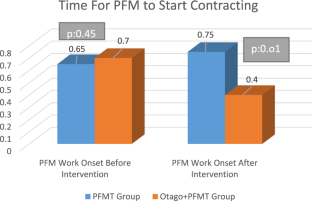
The median age of the IG (n: 22) and CG (n: 21) was 73.5 and 77 years, respectively. At baseline and after the intervention within the group, a significant improvement was observed in the PTDE-20 score (IG and CG, p: 0.00) and the 2-min step test in the IG (p: 0.02) and CG (p: 0.01). A significant decrease was found in the 2.45 m get up-and-go test, PFM work average onset, and PFM rest MVC EMG values (p: 0.01, p: 0.01, p: 0.00) in the IG. The PFM rest average value decreased (p: 0.04) in the CG.
Conclusion
The findings of this study show that combining PFMT with Otago exercises, two evidence-based interventions, is beneficial for effectively treating incontinence symptoms, balance and functional status in elderly people. Thus, a triple effect can be achieved with a single exercise training in the same treatment session and for the same duration.
Clinical trial number
Clinical trial number: NCT06331039.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save
Springer+ Basic
€32.70 /Month
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Buy Now
Price includes VAT (France)
Instant access to the full article PDF.
Rent this article via DeepDyve

Similar content being viewed by others

Pelvic floor muscle training, the risk of falls and urgency urinary incontinence in older women
Article 26 July 2021

Pelvic Floor Muscle Training for Older Women with Urinary Incontinence
Article 26 March 2020

Comparative analysis of pelvic floor muscle training and Pilates in managing urinary incontinence among postmenopausal women: a randomized controlled trial
Article 11 January 2024
Data availability
No datasets were generated or analyzed during the current study.
References
- Sk I (2007) Geriatric syndromes: Clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc 55:780–791 ArticleGoogle Scholar
- Kim H, Yoshida H, Suzuki T (2011) The effects of multidimensional exercise on functional decline, urinary incontinence, and fear of falling in community-dwelling elderly women with multiple symptoms of geriatric syndrome: a randomized controlled and 6-month follow-up trial. Arch Gerontol Geriatr 52(1):99–105 ArticlePubMedGoogle Scholar
- John G, Bardini C, Mégevand P, Combescure C, Dällenbach P (2016) Urinary incontinence as a predictor of death after new-onset stroke: A meta-analysis. Eur J Neurol 23(10):1548–1555 ArticleCASPubMedGoogle Scholar
- Değer TB, Saraç ZF, Savaş ES, Akçiçek SF (2019) The relationship of balance disorders with falling, the effect of health problems, and social life on postural balance in the elderly living in a district in Turkey. Geriatrics 4(2):37 ArticlePubMedPubMed CentralGoogle Scholar
- Moon S, Chung HS, Kim YJ et al (2021) The impact of urinary incontinence on falls: A systematic review and meta-analysis. PLoS ONE 16(5):e0251711 ArticleCASPubMedPubMed CentralGoogle Scholar
- World Health Organization (2020). Global Report on Falls Prevention in Older Age. 2007. https://www.who.int/ageing/publications/Falls_prevention7March.pdf?ua=1. Accessed 13 Jun 2022
- Ma Y, Li X, Pan Y et al (2021) Cognitive frailty and falls in Chinese elderly people: a population-based longitudinal study. Eur J Neurol 28(2):381–388 ArticleCASPubMedGoogle Scholar
- Arkkukangas M, Söderlund A, Eriksson S, Johansson A-C (2019) Fall preventive exercise with or without behavior change support for community-dwelling older adults: a randomized controlled trial with short-term follow-up. J Geriatric Phys Therapy 42(1):9–17 ArticleGoogle Scholar
- Moreno-Segura N, Igual-Camacho C, Ballester-Gil Y, Blasco-Igual MC, Blasco JM (2018) The effects of the pilates training method on balance and falls of older adults: a systematic review and meta-analysis of randomized controlled trials. J Aging Phys Act 26(2):327–344 ArticlePubMedGoogle Scholar
- Liew LK, Tan MP, Tan PJ et al (2019) The modified otago exercises prevent grip strength deterioration among older fallers in the Malaysian Falls assessment and intervention trial (MyFAIT). J Geriatric Phys Therapy 42(3):123–129 ArticleGoogle Scholar
- Stevens JA, Burns E (2020) CDC Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults, 3rd ed. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Atlanta, Georgia; 2015. https://www.cdc.gov/homeandrecreationalsafety/pdf/falls/CDC_Falls_Compendium-2015-a.pdf Accessed 13 Jun 2021
- Son N-K, Ryu YU, Jeong H-W, Jang Y-H, Kim H-D (2016) Comparison of 2 different exercise approaches: Tai Chi versus Otago, in community-dwelling older women. J Geriatric Phys Therapy 39(2):51–57 ArticleGoogle Scholar
- Jahanpeyma P, Kayhan Koçak FÖ, Yıldırım Y, Şahin S, Şenuzun AF (2021) Effects of the Otago exercise program on falls, balance, and physical performance in older nursing home residents with high fall risk: a randomized controlled trial. Euro Geriatric Med 12:107–115 ArticleGoogle Scholar
- Nelson ME, Layne JE, Bernstein MJ et al (2004) The effects of multidimensional home-based exercise on functional performance in elderly people. J Gerontol A Biol Sci Med Sci 59(2):M154–M160 ArticleGoogle Scholar
- Kim H, Suzuki T, Yoshida Y, Yoshida H (2007) Effectiveness of multidimensional exercises for the treatment of stress urinary incontinence in elderly community-dwelling Japanese women: a randomized, controlled, crossover trial. J Am Geriatr Soc 55(12):1932–1939 ArticlePubMedGoogle Scholar
- Cheng P, Tan L, Ning P et al (2018) Comparative effectiveness of published interventions for elderly fall prevention: a systematic review and network meta-analysis. Int J Environ Res Public Health 15(3):498 ArticlePubMedPubMed CentralGoogle Scholar
- Dumoulin C, Cacciari LP, Hay‐Smith EJC (2018) Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane database of systematic reviews (10).
- Virtuoso JF, Menezes EC, Mazo GZ (2019) Effect of weight training with pelvic floor muscle training in elderly women with urinary incontinence. Res Q Exerc Sport 90(2):141–150 ArticlePubMedGoogle Scholar
- Fisher S, Stanich S, Hong I et al (2019) Fall risk reduction in the elderly through the physical therapy management of incontinence. J Women’s Health Phys Therapy 43(1):3–9 ArticleGoogle Scholar
- Barber MD (2007) Questionnaires for women with pelvic floor disorders. Int Urogynecol J 18:461–465 ArticleGoogle Scholar
- Barber M, Walters M, Bump R (2005) Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 193(1):103–113 ArticleCASPubMedGoogle Scholar
- Toprak Ş. (2010) Pelvik Taban Distres Envanteri-20'nin Türkçe'ye Uyarlanması, Geçerlik ve Güvenirliği (tez). Ankara: Hacettepe Üniversitesi.
- Toprak CS, Akbayrak T, Kaya S, Ekici G, Beksac S (2012) Validity and reliability of the Turkish version of the pelvic floor distress inventory-20. Int Urogynecol J 23:1123–1127 ArticleGoogle Scholar
- Lucas M, Bosch R, Burkhard F et al (2013) European association of urology guidelines on assessment and nonsurgical management of urinary incontinence. Actas Urológicas Españolas (English Edition) 37(4):199–213 ArticleCASGoogle Scholar
- Garely AD, Noor N (2014) Diagnosis and surgical treatment of stress urinary incontinence. Obstet Gynecol 124(5):1011–1027 ArticlePubMedGoogle Scholar
- Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C (2005) Development and initial validation of the falls efficacy scale-international (FES-I). Age Ageing 34(6):614–619 ArticlePubMedGoogle Scholar
- Ulus Y, Durmus D, Akyol Y, Terzi Y, Bilgici A, Kuru O (2012) Reliability and validity of the Turkish version of the Falls Efficacy Scale International (FES-I) in community-dwelling older persons. Arch Gerontol Geriatr 54(3):429–433 ArticlePubMedGoogle Scholar
- Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47(11):1245–1251 ArticleCASPubMedGoogle Scholar
- Whitney SL, Poole JL, Cass SP (1998) A review of balance instruments for older adults. Am J Occup Ther 52(8):666–671 ArticleCASPubMedGoogle Scholar
- Sahin F, Yilmaz F, Ozmaden A, Kotevoglu N, Sahin T, Kuran B (2008) Reliability and validity of the Turkish version of the Berg Balance Scale. J Geriatric Phys Therapy 31(1):32–37 ArticleGoogle Scholar
- Rikli R.E. and Jones C.J., Senior fitness test manual. 2013: Human kinetics.
- Halski T., Słupska L., Dymarek R. et al (2014) Evaluation of bioelectrical activity of pelvic floor muscles and synergistic muscles depending on orientation of pelvis in menopausal women with symptoms of stress urinary incontinence: a preliminary observational study. BioMed research international 2014.
- Flury N, Koenig I, Radlinger L (2017) Crosstalk considerations in studies evaluating pelvic floor muscles using surface electromyography in women: a scoping review. Arch Gynecol Obstet 295:799–809 ArticlePubMedGoogle Scholar
- Péter A, Andersson E, Hegyi A et al (2019) Comparing surface and fine-wire electromyography activity of lower leg muscles at different walking speeds. Frontiers in physiology: p. 1283.
- Madill SJ, McLean L (2008) Quantification of abdominal and pelvic floor muscle synergies in response to voluntary pelvic floor muscle contractions. J Electromyogr Kinesiol 18(6):955–964 ArticlePubMedGoogle Scholar
- Chmielewska D., Stania M., Sobota G. et al (2015) Impact of different body positions on bioelectrical activity of the pelvic floor muscles in nulliparous continent women. BioMed Research International 2015.
- Madill SJ, McLEAN L (2007) A contextual model of pelvic floor muscle defects in female stress urinary incontinence: a rationale for physiotherapy treatment. Ann N Y Acad Sci 1101(1):335–360 ArticlePubMedGoogle Scholar
- Ptaszkowski K, Paprocka-Borowicz M, Słupska L et al (2015) Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: a preliminary observational study. Clinical interventions in aging: p. 1521–1528.
- Chen X, Zhao L, Liu Y et al (2021) Otago exercise programme for physical function and mental health among older adults with cognitive frailty during COVID‐19: a randomised controlled trial. Journal of Clinical Nursing.
- Davidson JE, Moore KH (2013) Pelvic floor muscle training for urinary incontinence in older adults: a systematic review. Australian and New Zealand Continence Journal, The 19(1).
- Bø K (2020) Physiotherapy management of urinary incontinence in females. J Physiother 66(3):147–154 ArticlePubMedGoogle Scholar
- Preparing the healthcare workforce to deliver the digital future. NHS Health Education England. [cited 19 April 2020.
- Li Y-T, Tsai Y-J, Wang L-Y, Ou Y-C, Kao Y-L, Lin K-Y (2023) The feasibility of a multimodal exercise program for sedentary postmenopausal women with urinary incontinence: a pilot randomized controlled trial. Maturitas 167:90–98 ArticlePubMedGoogle Scholar
- Wang Y, Yao J, Chen N, Liu J, Shi G, Wu Y (2022) Study of female pelvic floor muscle in overactive bladder based on MRI 3D reconstruction. BMC Urol 22(1):1–12 ArticleGoogle Scholar
- Abrams P, Andersson K-E, Birder L et al (2010) Fourth international consultation on incontinence recommendations of the international scientific committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn 29(1):213–240 ArticleCASPubMedGoogle Scholar
- Alves FK, Riccetto C, Adami DB et al (2015) A pelvic floor muscle training program in postmenopausal women: a randomized controlled trial. Maturitas 81(2):300–305 ArticlePubMedGoogle Scholar
- Madill SJ, Pontbriand-Drolet S, Tang A, Dumoulin C (2013) Effects of PFM rehabilitation on PFM function and morphology in older women. Neurourol Urodyn 32(8):1086–1095 ArticlePubMedGoogle Scholar
- Tosun O.C., Keser I., Dayican D.K., Yavuz O., Tosun G., and Kurt S. (2023) Does multiple-component intensive pelvic floor muscle training decrease muscle fatigue and symptoms in women with urinary incontinence? International Urogynecology Journal: p. 1–14.
- Alves JO, Da Luz ST, Brandão S, Da Luz CM, Jorge RN, Da Roza T (2017) Urinary incontinence in physically active young women: prevalence and related factors. Int J Sports Med 38(12):937–941 ArticlePubMedGoogle Scholar
- Sherburn M, Bird M, Carey M, Bø K, Galea MP (2011) Incontinence improves in older women after intensive pelvic floor muscle training: an assessor-blinded randomized controlled trial. Neurourol Urodyn 30(3):317–324 ArticlePubMedGoogle Scholar
Funding
1002 A rapid support program—Dokuz Eylül University Tubitak and Research universities support program, (ADEP).